Tissue Regeneration Through Cell Targeting
For gangrene and refractory skin ulcers, debridement (removal of necrotic tissue) is first performed, followed by surgery using pedicled flaps or free flaps to close the wound. However, this method often fails to completely reconstruct the original tissue, leaving scars and tissue defects, far from true regeneration.
In contrast, our research aims to develop scaffold materials that promote more natural wound healing, considering the quality of life (QOL), by simply placing them on the wound, without the need for tissue transplantation or suturing, allowing the tissue to integrate.
A New Form of Regenerative Medicine Without Transplants
Focusing on restoring local blood flow, we have succeeded in reconstructing vascular niches as sites for tissue regeneration. This technology is being considered for clinical applications in fields such as plastic surgery, dental and oral surgery, and dermatology.
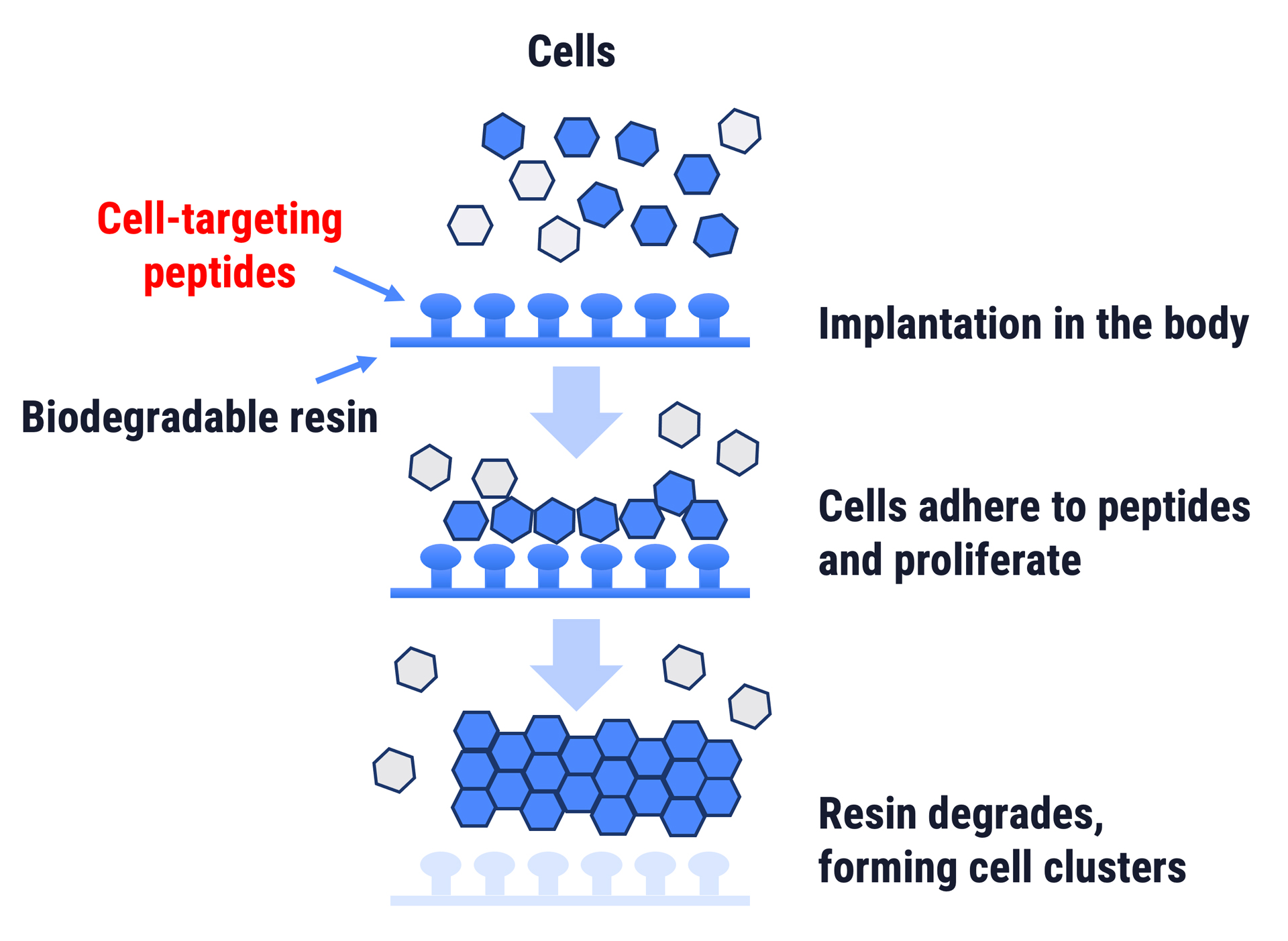
Specifically, from an embryological standpoint, we created bio-ink using a 3D bioprinter to express cell-targeting peptides on this scaffold material. This allows us to design tissue-specific vascular structures.
With this method, layered tissue regeneration progresses naturally, enabling “scarless wound healing” without hypertrophic scars or keloids. These studies aim to create scaffolds at CPC and conduct clinical trials.

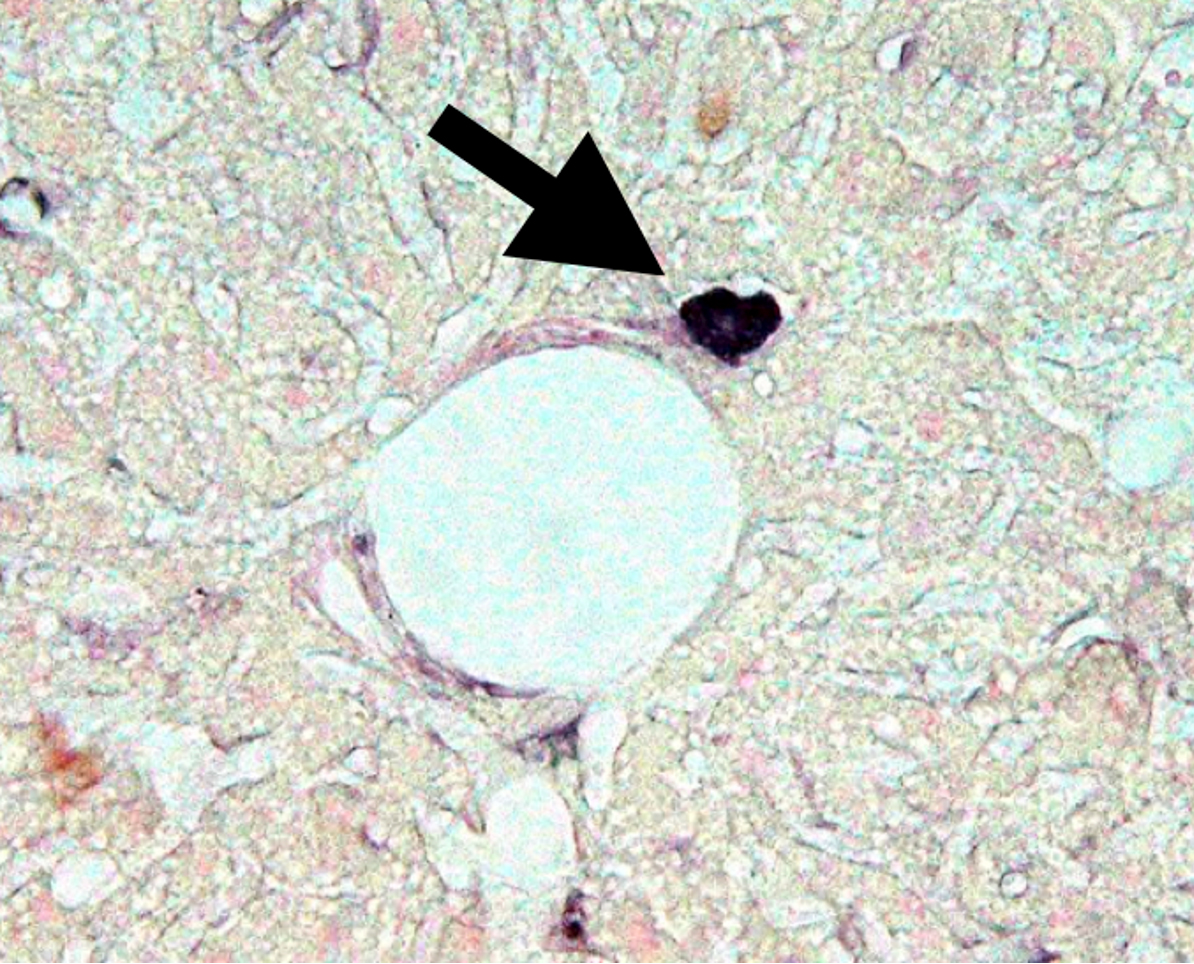
Discovery of the Cause of Diabetes
Abnormal cells causing diabetes and its complications discovered in hematopoietic stem cells.
Developing companion diagnostic drugs to diagnose diabetes based on the presence of diabetes stem cells in peripheral blood.
Biozipcode (Cell Targeting Technology)
An innovative system for delivering drugs exclusively to specific cells in the body.
Development of new drugs using Biozipcode and reuse of drugs previously unusable due to side effects.
Development of materials for tissue regeneration that can engraft onto tissues without needing transplants or sutures.